Stroke Thrombectomy Outcomes by Specialty: IRs vs. NIs
As we enter the third quarter of 2022, we are excited to share new stroke thrombectomy research, which even includes contributions from our very own interventional radiology team!
Our own interventional radiologist, Sabeen Dhand MD, contributed to this clinic research alongside a panopoly of distinguished practitioners, including:
- David Sacks, MD
- Ryan Hegg, MD
- Kevin Hirsch, MD
- Vance McCollom, MD
- Shawn Sarin, MD
- Venu Vadlamudi, MD
- Thomas Wasser, PhD
- Christopher Zylak, MD
Why this stroke thrombectomy treatment and oustudy?
This particular clinical study sought to better understand whether or not neurorinterventional physicians saw significantly higher success outcomes when performing stroke thrombectomy procedures, which, if false, would support making the procedure more widely available if offered by trained interventional radiologists as well.
As noted in the study, "endovascular interventions for large-vessel occlusion acute ischemic strokes are performed by interventional radiologists who have not undergone formal neurointerventional fellowship training.
There were no significant differences in the technical outcomes of procedure duration and successful revascularization or in the clinical outcome of return to independence between the specialties, as determined using both unadjusted and propensity score-matched analyses."
Widening the availability of stroke coverage and accessibility to stroke interventions has great implications on the future of health care!
How was the stroke research study performed?
The stroke study involved eight hospital institutions that offered both interventions for ischemic stroke by interventional radiologists as well as neurointerventional physicians. The data submitted was limited to the era of those performed with modern devices.
A total of 1,009 patient cases were submitted as part of the research study.
How was a successful stroke treatment outcome defined?
A 'good' clinical outcome, per this study, was defined as one that scored a 90-day modified Rankin score [mRS] of 0–2. Those cases must have achieved a technically-successful revascularization: a modified thrombolysis in cerebral infarction score of ≥2b.
By comparing outcomes between the specialties (after adjusting for treating hospital, patient age, stroke severity, Alberta stroke program early computed tomography score, time from symptom onset to door, and clot location), propensity score matching was used to compare the outcomes.
What was the outcome of the stroke thrombectomy study?
The results were groundbreaking!
They confirmed the original hypothesis: that treatment outcomes were not significantly different between those performed by IRs and NIs.

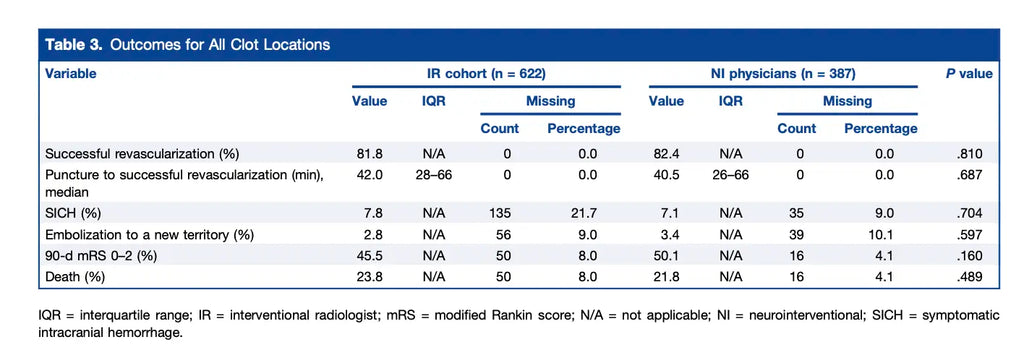
As notated above, the median time from stroke onset to puncture was 245 minutes for IRs versus 253 minutes for NIs (P = .49). The technically-successful revascularization rate was 81.8% for interventional radiologists versus 82.4% for neurointerventional physicians (P = .81). Along the same lines, the good clinical outcome rate was 45.5% versus 50.1% (P = .16).
After adjusting, the physician specialty was not a significant predictor of good clinical outcomes (odds ratio, 1.028; 95% confidence interval, 0.760–1.390; P = .86)! After matching, an mRS of 0–2 was present in 47.7% of IR treated patients and 51.1% of NI treated patients (P = .366).
Other key methodology takeaways:
As notated by the research, here are additional key takeaways in regards to its methodology:
- "The patients treated by IRs were significantly older than those treated by NI physicians (mean age, 71 vs 69 years; P = .02) but had similar stroke severity (NIHSS 17 vs 16; P = .26).
- Some records did not specify the branch or segment of the MCA (M1, M2, or M3/4). The IR-treated patients had a greater prevalence of MCA clots (75.4% vs 67.4%; P = .006) and a lower prevalence of basilar artery clots (6.4% vs 12.4%; P < .05) than the NI physician-treated patients.
- There were more left-sided clots in the IR-treated patients than in the NI physician treated patients, but the difference was not significant (54.8% vs 51.6%; P = .53).
- The median time from symptom onset to presentation was similar for IRs and NI physicians (165 vs 159 minutes; P = .60).
- The median time from door to puncture was similar for IRs and NI physicians (80 vs 63 minutes; P = .59).
- The median time from puncture to successful revascularization was nearly identical for IRs and NI physicians (42 vs 40.5 minutes; P = .69). The rates of successful revascularization (81.8% vs 82.4%, P =.81) and ENT (2.8% vs 3.4%, P =.81) were not statistically different.
- The SICH results were similar (7.8% vs 7.1%, P = .70).
- Some patients had missing data for ENT, SICH, and mRS. The results of these outcomes are summarized in Table 3:
What are physicians saying about EVT interventions in 2022?
Since a 2019 EVT study demonstrated the wide benefits of endovascular thrombectomy to treat large-vessel occlusion acute ischemic strokes (AIS), the practice has substantiated!
However, as the study notates, fewer than 6% of all AIS are treated with EVT.
As demand increases, so does hospitals' reliance on interventional physicians, including interventional radiologists and cardiologists, to perform endovascular thrombectomies. These physicians do not always have the same level of fellowship training as do nuerointerventional physicians.
While some posit that clinical outcomes will be lower if performed by those without this specialty training, this research suggests otherwise!
What are the weaknesses of this ischemic stroke study?
There were a few opportunities to even further bolster the integrity of this study's results, including:
- Implement a fully-randomized selection of physicians to perform the EVT procedures (the study, in some cases, deferred to the physician on-call, although no patient had their choice in the operating physician).
- Minimize selection bias by interventional radiologists who, in some cases, were deferred to to identify good candidates for the EVT procedure.
- Better normalize the study's selection criteria, as the NIs more often treated basilar occlusions, while the IRs more often treated M2 occlusions.
In conclusion
According to the CDC, more the 795,000 strokes occur each year in the United States alone. About 87% of these are ischemic strokes–those that block blood flow to the brain.
With greater prevalence of EVT to treat acute ischemic stroke for large-vessel occlusions, we can save many lives!
Want to read the full research study? You can read the full text in the Journal of Vascular and Interventional Radiology here:
Read the full stroke thrombectomy research study (2022)
Have any questions or would like to get in touch with our Southern California radiology teams?
Schedule an appointment or give us a call today!
Sources:
https://www.jvir.org/article/S1051-0443(22)00060-4/fulltext
https://www.cdc.gov/stroke/facts.htm
https://jnis.bmj.com/content/12/4/356

